DIELLI EXCLUSIVE INTERVIEW WITH PHYSICIAN OF INTERNAL MEDICINE AT ILLINOIS NORTHSHORE UNIVERSITY:-“Healthcare workers continue to be incredible examples of courage, empathy, and collegiality”-
by Rafaela Prifti-
In an exclusive interview with Adela K., Physician at Northshore University Healthsystem in Evanston Illinois, she detailed the current surge and demands on hospital capacities in the days leading to Thanksgiving holiday. She said that “for healthcare workers, even the most mundane tasks have turned into logistical nightmares from arranging reliable childcare, adding new steps to self-disinfecting after the work shift, maintaining social distance even when they go home, finding time for grocery shopping and meal preparation, helping children with remote learning all the way to their heightened sense of urgency in addressing issues such as advance directives and living wills.” Faced with extreme physical and mental exhaustion, “healthcare workers continue to be incredible examples of courage, empathy, and collegiality”
As a physician of the Department of Internal Medicine at Illinois Northshore University, what data do you have that indicates the severity of the current surge of the pandemic and how does it compare with the previous one?
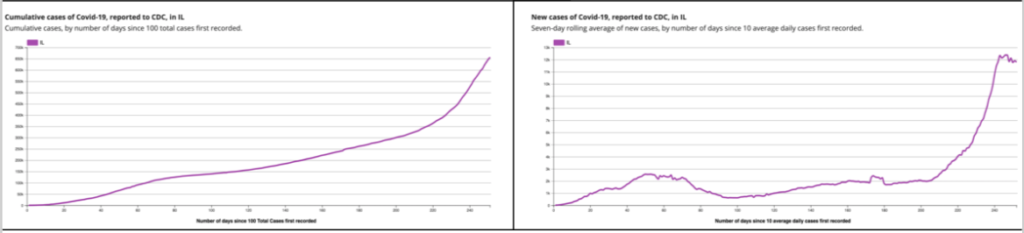
There has been a steady increase of cumulative cases in Illinois since the start of the pandemic as data provided by CDC recording the metric of cumulative cases of Covid-19 by number of days since 100 total cases first recorded, as shown in Graph 1. The number of new cases in the state is detailed in Graph 2. As of November 23, the number of infections statewide has totaled 664,620, and 11,552 Covid-19 related deaths. In my view, the severity of the surge correlates best with the number of new cases, the positivity rate, indicated in Graph 2 and other metrics such as mortality rate and the capacity of the healthcare system to handle the demands. Last week Illinois was averaging 12,384 new cases per day, the highest 7-day average since the start of the pandemic. This past week, luckily, we have seen a slight improvement from that number down to 8,322 of new confirmed and probable cases of COVID-19 on Monday Nov 23rd. But it is too early to tell if this is true bending of the curve or just a statistical fluctuation. And there’s the threat of holiday gatherings that can quickly undo any improvement.
The next three pictures provide a comparative view as they list the number of cases, deaths, total number of tests and test positivity given as cumulative count as well as in the last month and last week. The data shows that the positivity rate is at above 10 % this past month and past week, not quite as high as it was in the spring when it was above 20 %, but that is a reflection of more people being tested. The worst month in terms of deaths was May, with around 3000 deaths. On the bright side, we have learned a lot about SARS-CoV-2 and its management, so the death rate from the disease is lower now compared with the spring. That being said the cumulative number of SARS-Co-V-2 patients is much higher and therefore we are seeing the number of deaths increasing.
What about the capacity of the healthcare system to handle the current demand?
In terms of the capacity of the healthcare system to handle the demand, Chicago Tribune published an article to describe the situation in detail as of November 24. Here’s a chart showing the number of hospitalizations over time.
The guidance and advice of the public health officials is to break away from the traditional Thanksgiving gatherings in order to keep the holiday from having a negative impact on the current situation with the pandemic. What do you hear from your patients?
I practice in the inpatient setting. Since my patients are sick enough to be hospitalized, Thanksgiving travel plans are out of the question. We do recommend that after discharge, they continue to isolate for 20 days since the day of the positive test.
With consideration to the impact of the pandemic, some studies have focused on the connection between anxiety and mental illness and COVID-19:. I read some news reports about “long-haulers”? What can you tell us about it?
My practice is limited in the hospital setting. During the hospitalization period we do see a lot of encephalopathy which manifests as lethargy and confusion which are neurologic manifestations of Covid-19. Most people do improve by the time they are ready to be discharged, but I have seen a few cases of elderly who got sick in the spring, and have returned for different issues still not recovered mentally. It is a picture very similar to that of advanced dementia, some with behavioral disturbances. They require significant assistance with the activities of daily living. Then there is the separate group of the so-called “long haulers” who in addition to the physical symptoms experience significant anxiety and depression. There is a ripple effect in the society as a whole when we consider the impact the pandemic is having on the mental health of family members, associated with a significant level of stress compounded by limitations in visitation policies. I see a lot of anxiety, feeling of helplessness and being overwhelmed.
You mentioned that you will be in the Covid team for the next several days. Explain what that means, please.
We rotate as attending physicians for Covid patients. So in the next few days all my patients will be Covid patients who are hospitalized. I am part of the team that will be handling their management on the general medical floor.
For months now, one group, in particular, has been overwhelmed and overburdened to the brink of endurance. What can you tell us about the general mood of the health workers?
This is such a loaded question. For healthcare workers dealing with challenges and crisis has always been a daily occurrence. But the magnitude of this pandemic has faced health workers literally with the fight of their lives. In addition to the physical and mental demands of the job, there are new and significant challenges in our personal, family and social lives.
For us as essential workers who can not work from home, even the most mundane tasks all of a sudden have turned into logistical nightmares. Things like arranging reliable childcare, adding new steps to self disinfecting after work, maintaining social distance even within the home, finding time for grocery shopping and meal preparation, helping our children with remote learning, the list goes on. Even though most people I know avoid talking about it, especially in households where both parents are healthcare workers with young children, there is a heightened sense of urgency in addressing issues such as advance directives and living wills.
This pandemic is far from over and we have to keep going. Despite the physical and mental exhaustion they face, healthcare workers continue to be incredible examples of courage, empathy, and collegiality.